 ATC
ATC

Lifestyle decisions are much more important in determining who gets cancer and who does not.
Even if your genes place you at risk for cancer, 60% to 70% of all malignancies can be avoided by paying attention to 4 lifestyle factors:
-
Diet – Eating a plant-based diet is the single most important thing you can do to lower your cancer risk. Foods should be minimally processed and as close to their natural state as possible. Processed foods may have lost some of their nutritional value e.g. eat a plantain rather than plantain chips. Also limit intake of foods with added sugar, such as soft drinks and sweetened cereals. If you eat red meat, have no more than three ounces per day. Eating at least five servings—about one-half cup each—of fruits or vegetables every day can decrease your risk of cancer by 20%.
-
Weight control –Try not to gain too much weight after reaching your full height (at about age 18 for women... 24 for men).
-
Physical activity – Start by walking every day—working your way up to a brisk, one-hour walk daily. In addition, work up a sweat by engaging in some form of vigorous physical activity for at least one hour each week.
-
Not smoking and not drinking – Do not smoke. If you do drink, limit your consumption to one drink a day for women... two drinks a day for men. Drink alcohol in moderation, if at all.
CANCER RISK FACTORS
-
Family history of cancers, such as breast, ovarian and colon cancers.
-
Inflammatory bowel disease.
-
Human papillomavirus (HPV) infection.
-
Alcoholism.
-
Hepatitis B or C virus (HBV/HCV).
Additional risk factors for women...
-
First menstrual period before the age of 12.
-
First child born after age 30.
-
Childless and over age 50.
-
Post menopausal and on hormone-replacement therapy.
COLON CANCER AND PREVENTION
Tumors in the colon—and rectum—usually begin as tiny mushroom-shaped growths. Most of these polyps are harmless, but a small percentage turns cancerous. The progression from benign polyp to cancerous tumor takes at least five years. That's ample time for detecting and removing any polyps before they threaten your health.
If cancer cells are detected in the colon, removal of the polyps is curative in 92% of all cases.
Unfortunately, most people do not undergo the periodic screenings necessary to check the colon for growths.
-
Have periodic colonoscopies. Colonoscopy is an outpatient procedure in which a long, flexible viewing tube inserted through the rectum is used to examine the entire length of the large intestine. If polyps or tumors are detected, they often can be removed on the spot-the colonoscope doubles as a cutting tool.
If
you're
in good health
and
have
no family
history
of colon
cancer,
ask
your doctor
about having
a colonoscopy
once
every
5 to
10 years,
starting
at age 50.
If you have a family history of colon cancer, have your first colonoscopy no later than age 40... and perhaps even earlier.
The starting age—and the frequency of exams depend on how many of your first-degree relatives had colon cancer... and the age when it was diagnosed.
A
first-degree
relative
is a parent,
sibling
or child.
Ask your
doctor
which
schedule
is right
for you.
-
Consume at least 25g of dietary fiber a day. Fiber binds to special digestive juices known as bile acids in the intestine and carries them out of the body in the stool.
It
is more
effective
to
have
at least five servings
a day of fruits,
vegetables,
beans,
peas and whole
grains
e.g.
Yellow,
orange
and dark-green
vegetables
such as spinach
(tete),
oha and
ugu leaves,
whole
grains
such
as
wheat,
oats
and millet
and fruits
rich
in
Vitamins
A and
C.
Peppers,
beans,
broccoli
and cauliflower
are
rich
in vitamin
E,
folic acid
and
selenium.
Colon cancer occurs much less often in parts of the world where people eat lots of plant-based foods. Fiber is found only in plant foods.
-
Eat less fat. Reducing fat consumption to 20% of total calories is ideal. If that level is unrealistic for you, keep your fat intake under 30% of total calories. That means roughly 45g of fat a day. Cutting back on or eliminating red meat, butter and snack foods—and switching to non-fat dairy foods— is often enough to lower fat to the right level.
-
Don't eat charred meats. When animal fat is exposed to barbecuing with charcoal or to a direct flame in the broiler, carcinogens like those in tobacco are created.
-
Eat fish frequently Get 1,000 to 1,500mg of calcium a day. Three servings of low-fat milk or other dairy foods supply about 1,000mg. Calcium fights colon cancer by preventing rapid growth of cells in the colon.
PROSTRATE CANCER: WHAT EVERY MAN MUST KNOW
For such a small gland, the prostate causes big trouble. The disease kills almost as many men as breast cancer kills women.
SCREENING IS ESSENTIAL
Little is known about what causes prostate cancer, although men who eat a high-fat diet seem to be at greatest risk. Caught in its early stages, prostate cancer can usually be cured with surgery or radiation, and possibly helped by drug therapy. Key, of course, is catching the tumor before it spreads.
Once a year, starting at age 50 men should undergo:
-
Digital rectal examination (DRE). They insert a finger into the rectum to feel the prostate gland for nodules or firmness suggestive of cancer.
-
Prostate-specific antigen test. This measures blood levels of prostate-specific antigen (PSA), a protein secreted by the prostate. Elevated PSA levels suggest the need for further evaluation.
It’s important to realize that PSA levels increase with age. A level that's normal for a man of 80, for instance, may suggest prostate cancer in a man of 45.
*Start screenings at age 40 if your father or brother had prostate cancer. Risk is significantly higher among these men.
GETTING A PROPER BIOPSY
If your PSA is high, or if the digital exam reveals a suspicious lump, it's prudent to have the prostate biopsied. To be sure to find any tumor (and to estimate its size), however, the doctor must take at least six tissue samples. If tests indicate that the tumor is small and slow growing, treatment may be unnecessary.
If
PSA
levels
stay
low and the
tumor
grows
slowly,
"watchful
waiting"
may
be appropriate.
All you
must
do is have
a checkup
every
two
month,
including
a digital
rectal
exam
DRE
and PSA
test.
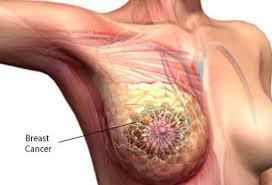
BREAST CANCER RISK FACTORS
-
Aging: On average, women over 60 are more likely to be diagnosed with breast cancer. Only about10 –15 percent of breast cancers occur in women younger than 45. However, this may vary for different races or ethnicities.
- Gender: Although nearly 2,000 men will be diagnosed with breast cancer each year, breast cancer is 100 times more common in women
- Family history: Having a family history of breast cancer, particularly women with a mother, sister or daughter who has or had breast cancer, may double the risk.
- Inherited factors: Some inherited genetic mutations may increase your breast cancer risks. Gene testing reveals the presence of potential genetic problems, particularly in families that have a history of breast cancer
- Obesity: After menopause, fat tissue may contribute to increases in estrogen levels, and high levels of estrogen may increase the risk of breast cancer. Weight gain during adulthood and excess body fat around the waist may also play a role.
- Not having children: Women who have had no children, or who were pregnant later in life (over age 35) may have a greater chance of developing breast cancer. Breast-feeding may help to lower your breast cancer risks.
- High breast density: Women with less fatty tissue and more glandular and fibrous tissue may be at higher risk for developing breast cancer than women with less dense breasts.
- Certain breast changes: Certain benign (noncancerous) breast conditions may increase breast cancer risk.
- Menstrual history: Women who start menstruation at an early age (before age 12) and/or menopause at an older age (after age 55) have a slightly higher risk of breast cancer. The increase in risk may be due to a longer lifetime exposure to the hormones estrogen and progesterone.
- A sedentary lifestyle: Physical activity in the form of regular exercise for four to seven hours a week may help to reduce breast cancer risk.
- Heavy drinking: The use of alcohol is linked to an increased risk of developing breast cancer. The risk increases with the amount of alcohol consumed.
- Birth control pills: Using oral contraceptives within the past 10 years may slightly increase the risk of developing breast cancer. The risk decreases over time once the pills are stopped.
- Combined post-menopausal hormone therapy (PHT): Using combined hormone therapy after menopause increases the risk of developing breast cancer. Combined HT also increases the likelihood that the cancer may be found at a more advanced stage.
- Diethylstilbestrol exposure (DES): Previous use of DES, a drug commonly given to pregnant women from 1940 to 1971 to prevent miscarriage, may slightly increase the risk of developing breast cancer. Women whose mothers took DES during pregnancy may also have a slightly higher risk of breast cancer.
- Radiation exposure: Women who, as children or young adults, had radiation therapy to the chest area as treatment for another cancer have a significantly increased risk for breast cancer.
Forty percent of diagnosed breast cancers are detected by women who feel a lump, so establishing a regular breast self-exam is very important. ͟While mammograms can help you to detect cancer before you can feel a lump, breast self-exams helps you to be
familiar with how your breasts looks and feels so you can alert your health care professional if there are any changes.
Though mammograms can often show a breast lump before it can be felt, a change in lifestyle will help reduce your risks of breast cancer.
