 ATC
ATC

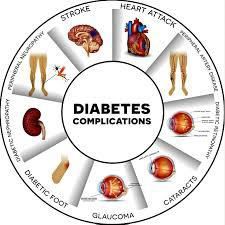
Diabetes is one of the most common chronic and serious ailments. It is the leading cause of both blindness and kidney failure. It can cause nerve damage that requires amputations. It also greatly raises the risk for heart disease and stroke.
The Two Types of Diabetes
Type 1 diabetes appears most often by young adulthood. But this type (once called juvenile-on set diabetes) accounts for only 5% to 10% of diabetic patients.
Type 2 diabetes strikes 8% to 10% of adults at sometime in their lives. While Type 2 usually develops after age 45, half of all people with the disease develop it before age 60.
Both kinds of diabetes involve elevated blood sugar levels, along with abnormal metabolism of fat and protein.
In Type 2 diabetes—which is often associated with obesity—the beta cells fail to make enough insulin. Because Type 2 diabetics may not need insulin shots, many people wrongly assume that the disease is not serious.
The onset of Type 1 diabetes is usually obvious. Common symptoms include extreme thirst, frequent urination, blurred vision or un-explained weight loss.
With Type 2, glucose levels rise so slowly that these symptoms take longer to show up or develop so gradually that they're noticed only after complications start to occur.
Half of the people suffering from Type 2 diabetes do not even know they have it. The longer diabetes goes untreated, the greater the risk of complications.
NOTE: In its early stages, type 2 diabetes causes only subtle symptoms.
Muscle fatigue, increased thirst and/or hunger, frequent urination, weight loss, blurred or double vision, anxiety, faintness or irritability.
If you suspect you have diabetes, ask your doctor about having a blood glucose test. This in-office test checks your glucose level before and after eating. You probably have diabetes if your fasting blood sugar level exceeds 126 or if your blood sugar level after eating exceeds 200.
Blood sugar is normally regulated by insulin, an enzyme synthesized by beta cells in the pancreas.
Testing Guidelines
The current universally accepted testing guidelines all adults age 45 or older to be screened for diabetes at least once every three years.
When Testing Reveals Diabetes
Adopt a low-carbohydrate diet.
You can eat liberal amounts of fowl, fish, cheese, eggs, green vegetables (including green leaf, water leaf spinach (efo and tete) and uguand oha leaves), cabbage, avocado, mushrooms, peppers, almonds, cashew nuts, walnuts etc.
Avery-low-carbohydrate
diet should be under taken only with a doctor's help. The doctor
should carefully monitor your cholesterol and triglyceride levels and
your kidney function until cholesterol and blood sugar levels are
acceptable.
Get aerobic exercise every day. Walking, bicycling, swimming or jogging— or doing some other form of aerobic exercise—for at least 30 minutes a day is even more important for diabetics than for non-diabetics.
Be vigilant about blood sugar testing. During the initial stages of diabetes treatment, when glucose levels are still fluctuating, doing a finger-stick blood testing is recommended just before and two hours after your morning and evening meals i.e. 4x daily.
Even more frequent testing may be helpful if blood sugar levels are not optimal.
Getting the Best Treatment
Caught early, Type 2 diabetes can often be controlled with diet and exercise alone.
80% of Type 2 diabetics are overweight. Once these patients lose weight blood sugar level and metabolic state improve.
The best way to do this is to cut back saturated fats and to boost consumption of grains, fruits and vegetables. Exercise also reduces the body's insulin needs by boosting the cells' sensitivity to insulin. To get started, go for a 20-minute walk each evening or take the stairs instead of the elevator at work, while shopping, etc.
The Best Fruits When You Have Diabetes
Berries – Almost all berries have a lesser impact on blood sugars than other fruit options. Berries are also loaded with vitamins and antioxidants. Add berries to yogurt, oatmeal, or blend in a protein-packed smoothie.
Citrus fruits – Fruits like grapefruit and oranges are high in fiber, which helps steady blood sugar levels. They’re also packed with vitamin C, which helps to boost your immune system.
Pears – One medium-sized pear provides 6 grams of fiber—about 24% of the daily recommended amount for women under the age of 50.
Apples – This is another great high-fiber option that pairs well with high-protein foods like nuts, nut butter and cheese.
Stone fruits – Fruits like plums, and peaches are generally low on the glycemic index when eaten fresh. Limit dried varieties, which makes their glycemic load substantially increase.
Grapes – grapes are a great source of fiber and vitamin B-6, which helps support brain function mood. One serving of about 15 grapes is all you need to get these health benefits without going overboard on carbohydrates.
Which Fruits Have the Most Sugar?
Mangoes - One mango has a whopping 45 grams of sugar -- not your best choice if you’re trying to watch your weight or how much sugar you eat. Maybe enjoy a couple of slices and save the rest for later.
Grapes - A cup of these has about 23 grams sugar.
Cherries - A cup of them has 18 grams. Measure your snack beforehand so you know exactly how much sugar you’ll get.
Pears - One medium pear has 17 grams of sugar. Just put a few slices in some low-fat yogurt or on top of a salad.
Watermelon - A medium wedge of this treat has 17 grams of sugar. Just keep it to a slice or two.
Bananas - One medium banana has 14 grams sugar. If that seems like more than you bargained for, slice half of it into your morning cereal or smash a small piece in the middle of your peanut butter sandwich.
Fruits with Less Sugar
Avocados – A whole avocado -- yep, it's a fruit -- has only half a gram of sugar. Put it in a salad, spread it on toast etc But while they’re low in sugar, they’re high in calories, so it might not be a good idea to make them a daily habit.
Guavas - Each one has 5 grams of sugar and about 3 grams of fiber, too -- more than you'd get from a serving of brown rice or a slice of whole-grain bread. You’ll get even more fiber if you add guavas with the skin on to your smoothies.
Raspberries - These are packed with 8 grams of fiber per cup -- and only 5 grams of sugar. The fiber is good for digestion and can help you feel fuller with fewer calories and they’re not bad with some fresh whipped cream and a spoon
Papayas - Half of a small one has 6 grams of sugar. Even a small one is pretty big, so half is plenty to eat at one time. You can add a squeeze of lime and a sprinkle of sea salt -- or a dollop of frozen yogurt for a tropical treat.
Strawberries - A cup of whole strawberries has only 7 grams. Add them to a salad for some vibrant color and a touch of summer.
As with any fruit, portion sizes and food pairings can be very important. Always stick to one serving size of fruit per meal to avoid excess carbohydrate intake.
The Fat You Eat and The Fat You Wear
Carrying excess body fat is the number-one risk factor for type 2 diabetes; up to 90 percent of those who develop the disease are overweight. What’s the connection? In part, a phenomenon known as the spillover effect.
Interestingly, the number of individual fat cells in your body doesn’t change much in adulthood, no matter how much weight you gain or lose. They just swell up with fat as the body gains weight, so when your belly gets bigger, you’re not necessarily creating new fat cells; rather, you’re just cramming more fat into existing ones. In overweight and obese people, these cells can get so bloated that they actually spill fat back into the bloodstream, potentially causing the same clogging of insulin signaling one would experience from eating a fatty meal.
Doctors can actually measure the level of freely floating fat in the bloodstream. Normally, it’s between about one hundred and five hundred micromoles per liter. But people who are obese have blood levels between roughly six hundred and eight hundred. People eating low-carb, high-fat diets can reach the same elevated levels. Even a trim person eating a high-fat diet can average eight hundred, so that sky-high number isn’t exclusive to obese patients. Because those eating high-fat diets are absorbing so much fat into their bloodstreams from their digestive tract, the level of free fat in their blood is as high as someone who’s grossly obese.
People who eat a plant-based diet, on the other hand, have just a small fraction of the rate of diabetes seen in those who regularly eat meat.
Saturated Fat and Diabetes
Not all fats affect our muscle cells in the same way. For example, palmitate, the kind of saturated fat found mostly in meat, dairy, and eggs, causes insulin resistance. On the other hand, oleate, the monounsaturated fat found mostly in nuts, olives, and avocados, may actually protect against the detrimental effects of the saturated fat.
Saturated fats can wreak all sorts of havoc in muscle cells and may result in the accumulation of more toxic breakdown products (such as ceramide and diacylglycerol) and free radicals and can cause inflammation and even mitochondrial dysfunction—that is, interference with the little power plants (mitochondria) within our cells. This phenomenon is known as lipotoxicity (lipo meaning fat, as in liposuction). If we take muscle biopsies from people, saturated fat buildup in the membranes of their muscle cells correlates with insulin resistance.
Monounsaturated fats, however, are more likely to be detoxified by the body or safely stored away.
Reversing Diabetes
As noted earlier, those with type 2 diabetes are at elevated risk for such serious health problems as heart disease, kidney disease, blindness, amputations, high blood pressure and stroke….
And the higher people’s blood sugar levels, the more heart attacks and strokes they tend to have, the shorter their life spans are, and the higher their risk of complications are.
Considering
that type 2 diabetes is a disease of insulin resistance, high blood
sugar is just a symptom of that disease, not the disease itself. So
even by artificially forcing down blood sugars by any means
necessary, we aren’t actually treating the cause—just like blood
pressure–lowering drugs aren’t actually treating the cause. By
lowering one of the disease’s effects, however, scientists hoped
they could prevent some of its devastating complications. The results
of this study, published in the New England Journal of Medicine, sent
shock waves through the medical community. The intensive
blood-sugar-lowering therapy actually increased subjects’
mortality, requiring the researchers to halt the study prematurely
for safety reasons. The drug combinations may have been more
dangerous than the high blood sugars they were trying to treat.
Insulin
treatments themselves may accelerate aging, worsen diabetic vision
loss, and promote cancer, obesity, and atherosclerosis. Insulin can
promote inflammation in the arteries, which may help explain the
increased death rate in the intensively treated group. So rather than
trying to overcome insulin resistance by brute force—just pumping
in more and more insulin—isn’t it better to treat the disease
itself by eliminating the unhealthy diet that caused it? That reminds
me of people who undergo bypass surgery for clogged arteries. If they
keep eating unhealthy, their bypasses will eventually get clogged
too. It’s better to treat the cause than the symptoms.
Once
again, researchers designed a study to uncover the answer. They
compared diabetics placed on the same postoperative diet before and
after they actually had the surgery. Amazingly, they found that the
diet alone worked better than the surgery even in the same group of
patients: The subjects’ blood sugar control was better in the
absence of the operation. This means the benefits of major surgery
may be obtained without you ever having to go under the knife and
getting your internal organs rearranged.
The bottom line: Blood sugar levels can normalize within a week of eating six hundred calories daily, because fat is pulled out of the muscles, liver, and pancreas, allowing them to function normally again. This reversal of diabetes can be accomplished either by voluntary calorie restriction or involuntarily, by having most of your stomach removed, a form of compulsory food restriction.
Undergoing surgery may be easier than starving yourself, but major surgery carries major risks, both during the operation and afterward. These risks include bleeding, leakage, infections, erosions, herniation, and severe nutritional deficiencies.
Surgery or starvation? There’s got to be a better way, and, in fact, there is. Instead of changing the quantity of food you eat, it’s possible to reverse diabetes by changing the quality of that food.
