 ATC
ATC
INFECTIONS CAN KILL: BE AWARE!!!
Humanity’s dominion over animals has unleashed a veritable Pandora’s ark of infectious diseases. Most modern human infectious diseases were unknown before domestication led to a mass spillover of animal disease into human populations. For example, tuberculosis appears to have been originally acquired through the domestication of goats but now infects nearly one-third of humanity. Meanwhile, measles and smallpox may have arisen from mutant cattle viruses. We domesticated pigs and got whooping cough, we domesticated chickens and got typhoid fever, and we domesticated ducks and got influenza. Leprosy may have come from water buffalo and the cold virus from horses. How often did wild horses have the opportunity to sneeze into humans’ faces until they were broken and bridled? Before then, the common cold was presumably common only to them. Once pathogens jump the species barrier, they can then transmit person-to-person. HIV, a virus thought to have originated from the butchering of primates in Africa for the bush-meat trade, causes AIDS by weakening the immune system. The opportunistic Fungal, viral, and bacterial infections AIDS patients contract—but to which healthy people are resistant—demonstrate the importance of baseline immune function. Your immune system is not just active when you’re lying in bed sick spiking a fever—it’s involved in a daily life-or-death struggle to save your life from the pathogens that surround and live inside you.

With every breath you take, you inhale thousands of bacteria, and with every bite you eat, you can ingest- millions more. Most of these tiny germs are completely harmless, but some can cause serious infectious diseases, occasionally making headlines with sinister-sounding names like SARS or Ebola. Although many of these exotic pathogens receive a lot of press coverage, more lives are lost to some of our most common infections.
Bear in mind that you don’t need to come in contact with a sick person to fall ill with an infection. There are latent infections that may exist within you, waiting to strike should your immune function falter. That is why it’s not enough to just wash your hands; you have to keep your immune system healthy.
Protecting Others
To protect others when you’re sick, you need to practice good respiratory etiquette by coughing or sneezing into the crook of your arm (into your bent elbow). This practice limits the dispersal of respiratory droplets and also avoids contaminating your hands. The Mayo Clinic has a slogan worth remembering: “The ten worst sources of contagion are our fingers.” When you cough into your hand, you can transfer contagion to everything from elevator buttons and light switches to gas pumps and toilet handles. It’s no surprise that during flu season, the influenza virus can be found on more than 50 percent of common household and day-care-center surfaces. Ideally, you should sanitize your hands after every bathroom visit and handshake, before all food preparation, and before touching your eyes, nose, or mouth after coming in contact with public surfaces. The latest recommendations from the World Health Organization favor the use of alcohol-based sanitizing rubs or gels over hand washing for routine disinfection of your hands throughout the day. (Products containing between 60 and 80 percent alcohol were found to be more effective than soap in every scientific study available for review.) The only time hand washing is preferable is when they are dirty or visibly contaminated with bodily fluids. For routine decontamination—that is, for all other times—alcohol-based products are the preferred method for hand sanitation. Still, some germs will always get past your first line of defense of practicing good hand hygiene. This is why you need to keep your immune system functioning at peak performance with a healthy diet and lifestyle.
Preventing Infectious Diseases with a Healthy Immune System
The term “immune system” is derived from the Latin word immunis, meaning untaxed or untouched, which is fitting, given that the immune system protects the body from foreign invaders. Composed of various organs, white blood cells, and proteins called antibodies that form alliances against trespassing pathogens threatening the body, the immune system, apart from the nervous system, is the most complex organ system humans possess.
Your
first layer of protection against intruders is physical surface
barriers like your skin. Beneath that are white blood cells. As you
get older, though, your immune function declines. Is this just an
inevitable consequence of aging? Or could it be because dietary
quality also tends to go down in older populations? To test the
theory that inadequate nutrition could help explain the loss in
immune function as you age, researchers split eighty-three volunteers
between sixty-five and eighty-five years old into two groups. The
control group ate fewer than three daily servings of fruits and
vegetables, while the experimental group consumed at least five
servings a day. They were all then vaccinated against pneumonia, a
practice recommended for all adults over the age of sixty-five. The
goal of vaccination is to prime your immune system to produce
antibodies against a specific pneumonia pathogen should you ever
become exposed. Compared with the control group, people eating five
or more servings of fruits and vegetables had an 82 percent greater
protective antibody response to the vaccine—and this was after only
a few months of eating just a few extra servings of fruits and
vegetables a day. That is how much control the fork may exert over
immune function. Certain fruits and vegetables may give the immune
function an extra boost.
You may have been taught as a kid to eat your veggies, including cruciferous ones like broccoli, kale, cauliflower, cabbage, and Brussels sprouts. But your parents probably didn’t tell you why you should eat them. Now we know that this family of vegetables contains compounds necessary for the maintenance of the body’s intestinal defenses. In short, broccoli is able to rally your immune system foot soldiers.
The
body uses up a lot of energy to maintain its immune system, so why
remain on high alert 24-7 when we only eat a few times a day? Why
would our bodies specifically use vegetables as the bat signal to
assemble the troops?
Vegetables’ presence in the gut works as a signal to upkeep our immune systems.
So if we don’t eat plants with each meal, we may be undermining our bodies’ strategy to protect us.
Interestingly, the immune boost provided by cruciferous vegetables like broccoli not only protects us against the pathogens found in food but also against pollutants in the environment. We’re all constantly being exposed to a wide range of toxic substances— other plants may also defend against toxic invaders. Researchers in Japan found that phytonutrients in such plant foods as fruits, vegetables, tea leaves, and beans can block the effects of dioxins in vitro.
For instance, the researchers found that having phytonutrient levels in the bloodstream achieved by eating three apples a day or a tablespoon of red onion appeared to cut dioxin toxicity in half.
The only catch was that these phytonutrient effects lasted only a few hours, meaning you may have to keep eating healthy foods, meal after meal, if you want to maintain your defenses against pathogens as well as pollutants.
Boosting the Immune System with Exercise
What if there was a drug or supplement that could halve the number of sick days you take due to such upper-respiratory infections as the common cold? It would make some pharmaceutical company billions of dollars. But there is already something that can boost your immune system for free and by so much that you can achieve a 25–50 percent reduction in sick days. And it has only good side effects. What is it? Exercise.
What’s more, it doesn’t take much of a workout to get results. Studies find that if you let kids run around for just six minutes, the levels of immune cells circulating in their blood increases by nearly 50 percent. At the other end of the life cycle, regular exercise can also help prevent age-related immune decline. One study found that while elderly, sedentary women have a 50 percent chance of getting an upper-respiratory illness during the fall season, those randomized to begin a half-hour-a-day walking program dropped their risk down to 20 percent. Among conditioned runners, though, the risk was just 8 percent. Exercising appeared to make their immune systems more than five times better at fighting infection.
While regular physical activity improves immune function and lowers respiratory infection risk, sustained and intense exertion may have the opposite effect. As you go from inactive to active, infection risk declines, but at a certain point, overtraining and excessive stress can increase the risk of infection by impairing immune function.
Food Poisoning
According to the Centers for Disease Control and Prevention CDC, roughly forty-eight million people are sickened annually. More than one hundred thousand of them are hospitalized, and thousands die, just because of something they ate.
In terms of healthy years of life lost, the top five most devastating pathogen-food combinations are Campylobacter and Salmonella bacteria in poultry, Toxoplasma parasites in pork, and Listeria bacteria in deli meats and dairy products. One of the reasons animal foods are the leading culprits is that most food-borne pathogens are fecal pathogens. Because plants don’t poop, the E.coli you may get from spinach didn’t actually originate in the spinach; E. coli is an intestinal pathogen, and spinach doesn’t have intestines. The application of manure to crops has been found to increase the odds of E. coli contamination by more than fiftyfold.
Salmonella is often the leading cause of food poisoning–related hospitalizations, as well as the number-one cause of food poisoning–related death. And it’s on the rise. Over the past decade, the number of cases has increased by 44%, particularly among children and the elderly. Within twelve to seventy-two hours after infection, the most common symptoms appear—fever, diarrhea, and severe abdominal cramps. The illness typically lasts between four and seven days, but among children and the elderly, the disease can be severe enough to require hospitalization— or funeral arrangements. Many people associate Salmonella with eggs—and for good reason. In 2010, for instance, more than half a billion eggs were recalled due to Salmonella outbreaks.
If proper cooking kills the bug, then why do hundreds of thousands continue to be sickened by Salmonella-contaminated poultry every year? The problem here is cross-contamination. Between the times the fresh or frozen bird is picked up from the store and when it’s slid into the oven, the germs on the chicken can contaminate hands, utensils, and kitchen surfaces. Studies have shown that up to 80 percent of the time, placing fresh chicken on a cutting board for a few minutes can transfer disease-causing bacteria. Then, if you put cooked chicken back on the same cutting board, there’s about a 30 percent chance that the meat will become re-contaminated.
Antibiotics Resistance
The Centers for Disease Control and Prevention (CDC) calls antibiotic resistance one of the biggest public health challenges of our time. Conservative estimates find at least 2 million are infected and 23,000 die each year with antibiotic resistant bacteria. When a germ develops the ability to withstand drugs designed to kill them, they become antibiotic-resistant and are called superbugs.
Antibiotic resistance happens naturally as bacteria adapt to drugs. Resistance is helped along by the inappropriate use of medications, such as antibiotics for viral infections and their use in agriculture. The World Health Organization warns emerging resistance to antibiotics threatens the ability to treat common infections that may result in prolonged illness, disability and death.
Simple medical procedures may become high risk, which means the cost of health care rises. In what researchers believed was the first national estimate of the cost for treating antibiotic-resistant infections, they found a national cost of $2.2 billion in 2014, having doubled since 2002.
Antibiotic resistance is a worldwide crisis with the potential to threaten people at any age. One bacterium known to be fatal to the elderly and sick is clostridium difficile, or C. diff. In a recent study it was reported that this bacterium has become highly adapted to spreading inside hospitals, and they may have found the reason why.
Clostridium difficile (C-diff) loves sugar and resists disinfectant
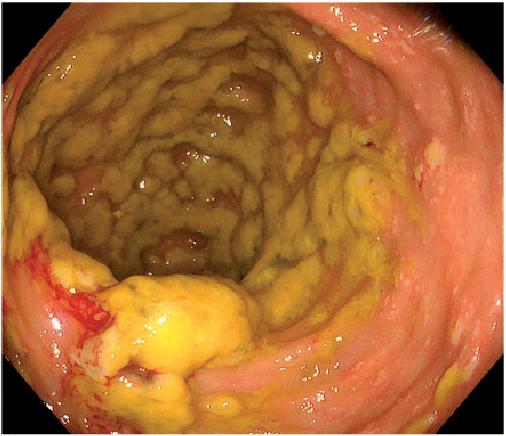
The Centers for Disease Control and Prevention reported that 15,000 die every year from Clostridium difficile (c-diff), a bacterium that may trigger watery diarrhea, fever, dehydration and kidney failure. It is evolving to a superbug, and has adapted to sugars commonly found in a Western diet. It also produces spores capable of resisting disinfectants
Antibiotics are what has turned this minor player, accounting for up to 3% of bacteria in normal flora, to a major health concern; when antibiotics disrupt the normal flora, harmful bacteria such as C. diff are able to thrive and spread in the environment
Hand-washing is the single most effective means of preventing the spread of infection and reducing your risk of needing antibiotics. Hand washing supports a strong gut microbiome, which is another means of prevention
Most people are aware of hand sanitizers that are advertised, they kill 99.99 percent of all germs. Well, C. diff falls into that 0.01 percent. They don’t call it a superbug for nothing. Residual spores of the pathogen have been shown to be readily transmitted with a handshake even after using hand sanitizer.
Bacteria and sugar make a deadly combination
A mild to moderate infection with this bacterium affects the gut, causing watery diarrhea for two to three days and mild abdominal cramping and tenderness.A severe infection can trigger diarrhea, fever, kidney failure, dehydration and weight loss.
The bacteria are now able to take advantage of high sugar diets and resist disinfection commonly used in the hospital. In a recent study researchers showed how C. diff can exist for long periods of time on disposable equipment and vinyl surfaces, even after having been cleaned with disinfectant.
C. diff is commonly found in the environment
According to Harvard Health, C. diff accounts for up to 3% of bacteria in a normal intestinal flora. Although present, it is usually harmless as good bacteria keep it under control.It turns out that antibiotics have turned this minor player into a major problem. Once antibiotics have disrupted the normal flora in your gut, this allows harmful bacteria to thrive, including C. diff. This in turn triggers diarrhea.
C. diff forms spores that may get into the environment through those who are infected, when they touch surfaces. When others touch the newly-contaminated surfaces and then touch their mouths, the infection spreads.
Health care workers may also spread the bacteria when their hands are contaminated. Since antibiotics alter the normal flora found in the intestinal tract, and a large number of patients receive antibiotics in health care settings, this can lead to C. diff outbreaks.
Poop pills may help combat an outbreak
C. diff can trigger a life-threatening condition in those who have been on antibiotics or have a compromised immune system. According to the CDC, there are 500,000 C. diff infections each year resulting in 15,000 deaths. One treatment methodology is a stool transplant, which has been used throughout history.
Although
new to Western medicine, fecal transplants were described as far back
as 1,700 years ago by a Chinese researcher who first used what he
called “yellow soup” to treat patients with severe diarrhea. In
World War II, the stools of camels were used to treat bacterial
dysentery in German soldiers.
In 1958, the treatment was described in a report for a patient with antibiotic-associated diarrhea. But it was not until 1978 that the value was recognized in the treatment of C. diff. The treatment goes under several different names including fecal biotherapy and fecal floral reconstitution.
Prevention is still the best medicine
The single most effective means to prevent the spread of infection is through hand washing. The CDC recommends cleaning your hands to prevent the spread of germs. However, they find on average health care workers do this less than half the time they should.
Thoroughly clean your hands and reduce to risk of transmitting disease.
A second preventive strategy includes protecting your gut microbiome from the effects of antibiotics. It is important to take antibiotics only when they're necessary. You should not use them for viral infections, which may contribute to the development of antibiotic resistance.
Antibiotics have no effect on viruses and you'll likely get greater relief by using a combination of natural remedies.
Support strong gut bacteria for good health
Supporting the growth of beneficial bacteria in your gut microbiome may affect your mental and physical health. Sugar is one of the most negative culprits because it contributes to a dysfunctional gut microbiome. A study published in January 2019, found that sugars affect a regulator of gut colonization for beneficial bacteria.
In essence, glucose and fructose turn off the expression of a protein regulating gut colonization by beneficial microbes. Sugar disrupts the generation of proteins that foster the growth of beneficial bacteria found in lean, healthy individuals.
Since gut dysfunction may lead to a system-wide inflammatory response, it is important to address the needs of your gut bacteria consistently. As a general rule, once you start healing your gut, you should start feeling better in a couple of weeks to a few months.
ADDITIONAL INFORMATION ON THE OVERUSE OF ANTI-BIOTICS
Dr. Margaret Chan, former Director-General of the World Health Organization, warned that we may be facing a future in which many of our miracle drugs no longer work. She stated, “A post-antibiotic era means, in effect, an end to modern medicine as we know it. Things as common as strep throat or a child’s scratched knee could once again kill.” We may soon be past the age of miracles. The director-general’s prescription to avoid this catastrophe included a global call to “restrict the use of antibiotics in food production to therapeutic purposes.” In other words, only use antibiotics in agriculture to treat sick animals. But that isn’t happening, in the RECENT TIMES Nigeria, meat producers feed millions of pounds of antibiotics each year to farm animals just to promote growth or prevent disease in the often cramped, stressful, and unhygienic conditions of industrial animal agriculture particularly poultry and fish farming.

Yes, physicians overprescribe antibiotics as well, but the there is a real possibility thatabout 80 percent of the antimicrobial drugs sold in the country every year now go to the animal farm industry. Antibiotic residues can then end up in the food you eat. Studies have revealed that traces of such antibiotics as Bactrim, Cipro, and Enrofloxacin have been found in the urine of people eating meat—even though none of them were taking those drugs. The researchers concluded: “Consumption amounts of beef, pork, chicken, and dairy products could explain the daily excretion amount of several antibiotics in urine.” These antibiotic levels can be lowered, however, after merely five days of removing meat from the diet.
Healthy living may help protect you against both airborne and foodborne illnesses. Eating more fruits and vegetables and exercising more frequently can boost your immune system to help you fight off respiratory infections like the common cold. And sticking to mostly plant foods can help prevent you from becoming another food poisoning statistic by reducing your exposure to some of the deadliest fecal pathogens.
